
Probiotics for IBS: What the Evidence Says
Living with Irritable Bowel Syndrome (IBS) can feel like a constant guessing game. One day you are fine, the next you are dealing with bloating, pain, or unpredictable bowel habits. If you are looking for a structured way to manage your symptoms, probiotics might be on your radar. But with so much conflicting information, where do you start?
This article provides a clear, evidence-based guide to using probiotics for IBS. We will look at the specific strains that have been studied, how to trial them effectively, and what UK health bodies say about their use.
The Evidence for Probiotics in IBS
The idea behind using probiotics is to support the balance of your gut microbiome, the community of trillions of bacteria living in your digestive tract. Research suggests that in some people with IBS, this balance may be disrupted. Re-introducing beneficial bacteria could help to restore order and ease symptoms.
However, not all probiotics are the same. The benefits are strain-specific, meaning different bacteria do different jobs. The British Society of Gastroenterology guidelines suggest that it is reasonable for people with IBS to try probiotics for up to twelve weeks, but only if they are discontinued if no improvement is seen.
Here are some of the most researched strains for different types of IBS.
For IBS with Constipation (IBS-C): Strains like Bifidobacterium longum have shown promise. Research has found that Bifidobacterium longum W11 helped to improve bowel frequency and reduce abdominal pain in people with IBS-C. This strain works by regulating key pathways involved in inflammation and supporting healthy bowel movements.
For IBS with Diarrhoea (IBS-D): Research has pointed to the effectiveness of Clostridium butyricum CBM588. This strain helps produce butyrate, a short-chain fatty acid that supports gut health and has been shown to improve stool consistency and quality of life in those with IBS-D. It is the only butyrate-producing probiotic currently available for medical use in Europe.
For General Symptoms (Pain and Bloating): Lactobacillus plantarum 299v (LP299V) is one of the most extensively studied probiotics for IBS. Multiple trials have found it can significantly reduce abdominal pain and bloating. A four-week treatment with LP299V provided effective symptom relief, particularly for these two symptoms.
Finding the right probiotic is a process of careful trial and error. The NHS advises trying a probiotic for at least four weeks to see if it helps. A structured approach is the best way to understand what works for you.
Here is a simple, four-step method to follow.
Step 1: Choose One Strain at a Time
Start with a single-strain probiotic that matches your main symptom. For example, if you have IBS-C, choose Bifidobacterium longum. If you have IBS-D, consider Clostridium butyricum. This helps you to isolate what is working. A multi-strain formula can be trialled later, but starting simple makes it easier to pinpoint cause and effect.
For a targeted, high-strength option, a multi-strain formula like Flora Max, which contains 20 billion CFU and includes several of the strains mentioned above, can be an effective choice once you have established that probiotics help you.
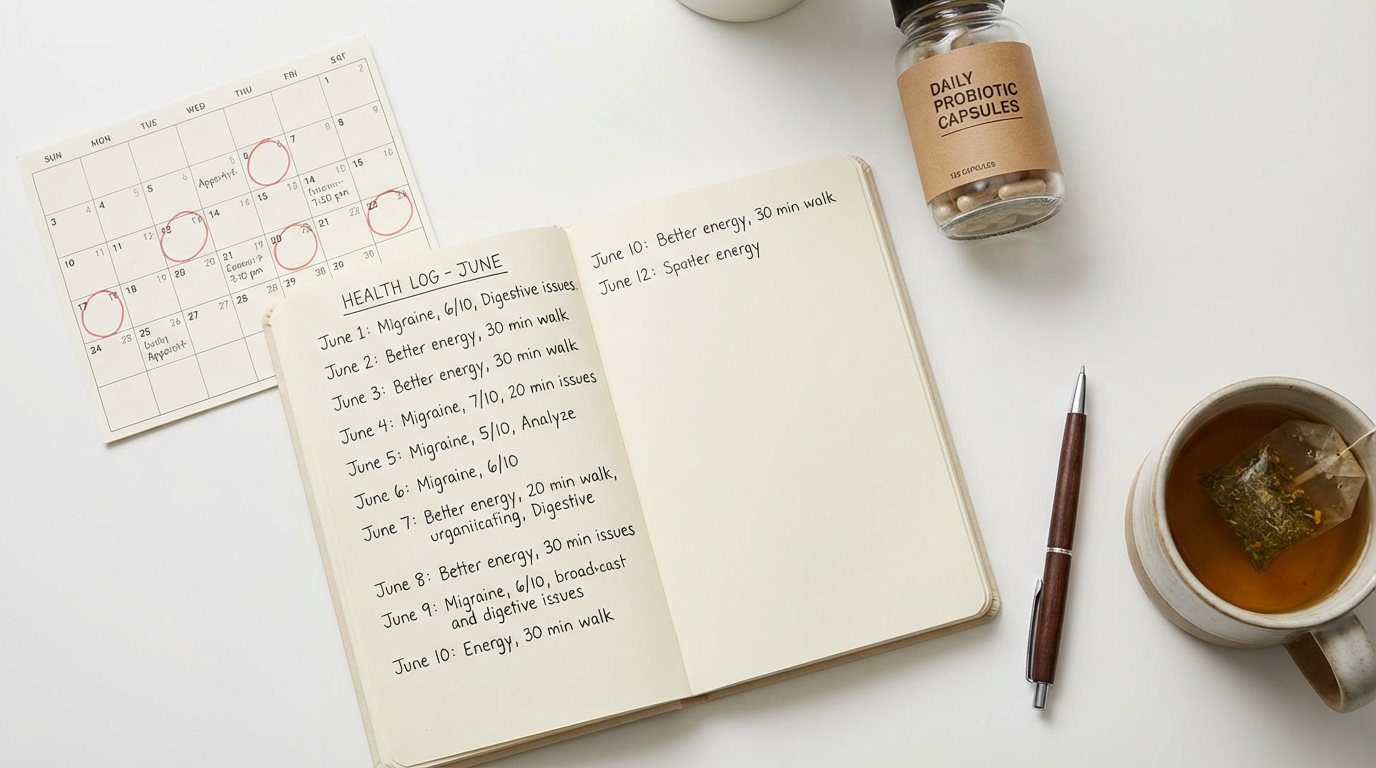
Step 2: Keep a Symptom Diary
For four to twelve weeks, take the probiotic daily and keep a simple diary. Note your key symptoms, such as bloating, pain, and bowel movements. Record the date, time, and severity of each symptom. This record will give you objective data to look back on, rather than relying on memory. You can use a simple notebook or a spreadsheet, whatever works best for you.
Step 3: Maintain a Consistent Diet
Try to keep your diet consistent during the trial period. This is not the time to also start a new diet like the low FODMAP diet. Combining too many changes makes it impossible to know what is responsible for any improvements. The low FODMAP diet is a separate, effective tool for managing IBS, but it should be done under the guidance of a professional and not at the same time as a probiotic trial.
Step 4: Review and Decide
After the trial period, review your diary. Have your symptoms improved? If so, you may have found a probiotic that works for you. If not, it is best to stop taking it and consider trying a different strain or seeking further advice from your GP or a dietitian.
For daily maintenance after you have found a probiotic that works, a product like Pro Flora provides a solid foundation. This contains 4 billion CFU, which is suitable for ongoing support.
Important Considerations
Probiotics are not a magic bullet for IBS, but they are a valid, evidence-based tool that can form part of a wider management plan. By taking a structured, methodical approach, you can discover if they are right for you without wasting time or money.
If you are considering a new supplement, and especially if you have a weakened immune system or are taking medications, it is always a good idea to speak with a healthcare professional first. They can advise on whether probiotics are suitable for your specific situation and whether they might interact with any medications you are taking.
For a closer look at our full range of digestive health supplements, you can browse our Probiotic Bacteria Supplements collection.

Leave a comment